Understanding Fibromyalgia Flare–Ups
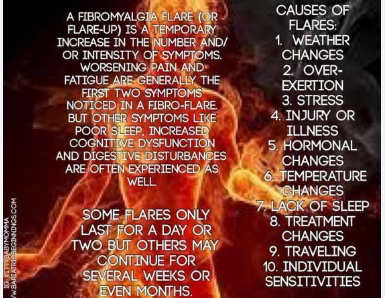
Fibromyalgia is a chronic condition characterized by widespread musculoskeletal pain, fatigue, and a variety of cognitive and emotional symptoms. While baseline symptoms may be present every day, many people experience periodic intensifications known as flare–ups. These episodes bring a sudden and severe worsening of symptoms that can last for days, weeks, or even longer.
Flare–ups can disrupt routines, affect mental health, and pose serious challenges for work and social life. Recognizing the symptoms of a fibromyalgia flare–up is essential for early intervention, effective management, and reducing long-term impact on health.
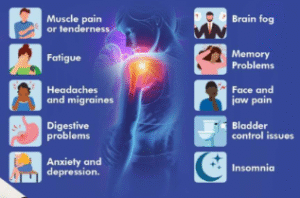
Sudden Increase in Widespread Pain
The most prominent symptom of a fibromyalgia flare–up is an increase in the intensity and spread of pain. This pain may feel like deep, aching soreness, stabbing sensations, or throbbing discomfort throughout the muscles and soft tissues. Pain may radiate to new areas or worsen in spots that are typically less affected during baseline periods.
This heightened sensitivity to pain, known as hyperalgesia, occurs due to central nervous system sensitization. Even mild physical contact or gentle movement can become unbearable during a flare.
Overwhelming Fatigue and Exhaustion
Fatigue during a fibromyalgia flare–up is not just ordinary tiredness. It is often described as a crushing, all-encompassing weariness that can make it difficult to get out of bed, concentrate, or perform the simplest tasks. This exhaustion can persist even after a full night’s sleep.
Unlike physical tiredness that improves with rest, flare–up fatigue resists recovery and may be worsened by exertion, stress, or poor sleep quality.
Brain Fog and Cognitive Dysfunction
Also referred to as “fibro fog,” cognitive dysfunction is a hallmark of flare–ups. Individuals may experience difficulty concentrating, poor memory, slow thinking, and confusion. Words may be hard to find, tasks take longer to complete, and mistakes become more frequent.
This mental cloudiness can be particularly frustrating for those who otherwise perform well cognitively, contributing to anxiety and reduced self-esteem.
Increased Sensitivity to Light, Sound, and Temperature
Sensory sensitivity becomes more pronounced during a fibromyalgia flare–up. Everyday sounds may feel overwhelmingly loud, lights too bright, or room temperatures uncomfortably hot or cold. This reaction is due to how the nervous system misinterprets external stimuli, leading to a state of sensory overload.
For many people, these triggers worsen other symptoms, creating a loop of discomfort that can be difficult to break.
Digestive Problems and Gastrointestinal Distress
Flare–ups often amplify gastrointestinal symptoms, such as bloating, abdominal cramps, constipation, or diarrhea. These issues are frequently related to irritable bowel syndrome (IBS), a condition that often coexists with fibromyalgia.
Stress, dietary changes, and disrupted sleep patterns during a flare can further aggravate digestive symptoms, creating a cycle of discomfort and dietary avoidance.
Mood Swings, Anxiety, and Depression
Fibromyalgia flare–ups are frequently accompanied by a surge in emotional symptoms. Anxiety, depression, mood swings, and irritability may intensify due to physical discomfort, reduced activity, and poor sleep.
The emotional toll can deepen feelings of isolation, especially when others do not understand the invisible nature of the condition. It becomes a challenge to maintain emotional stability when pain and fatigue dominate the experience.
Sleep Disturbances and Restless Nights
Sleep quality takes a noticeable hit during flare–ups. Many people report difficulty falling asleep, staying asleep, or feeling refreshed in the morning. Restless legs, night sweats, and frequent awakenings are also common.
Even when sleep occurs, it may lack the deep, restorative stages necessary for healing. This unrefreshing sleep worsens fatigue and cognitive issues, adding to the flare–up’s severity.
Tingling, Numbness, and Unusual Sensations
Neurological symptoms like tingling, numbness, and burning sensations may increase during a flare–up. These sensations often occur in the hands, feet, arms, or face and can be unsettling.
These symptoms are caused by the abnormal processing of nerve signals rather than actual nerve damage, reflecting the brain’s heightened sensitivity to internal messages.
Muscle Stiffness and Reduced Mobility
Stiffness often peaks during flare–ups, especially in the morning or after periods of inactivity. This can limit range of motion, delay mobility, and create difficulty with tasks such as dressing, walking, or climbing stairs.
This stiffness is not just muscle tightness but a systemic response to inflammation, disrupted sleep, and heightened pain sensitivity.
Heightened Reaction to Stress
Stress is both a trigger and a magnifier of fibromyalgia flare–ups. During a flare, the body’s reaction to stress becomes exaggerated. Minor challenges can feel overwhelming, and physical symptoms may worsen in response to emotional strain.
Managing stress becomes increasingly important during a flare, as elevated cortisol and other stress hormones can prolong and deepen symptoms.
Urinary Frequency and Bladder Discomfort
Some people experience an uptick in urinary symptoms during a flare, including increased urgency, frequency, and pelvic discomfort. These symptoms may mimic urinary tract infections but are often related to interstitial cystitis or bladder pain syndrome, which frequently overlaps with fibromyalgia.
Hydration, avoiding bladder irritants, and relaxation strategies may help reduce discomfort during flare–ups.
Chills, Sweating, and Thermoregulation Issues
Many individuals report feeling feverish, experiencing chills, or breaking into unexpected sweats during a fibromyalgia flare–up. These temperature regulation issues stem from autonomic nervous system dysfunction, which disrupts the body’s internal thermostat.
Even when there is no actual fever, the sensation of being hot or cold can cause significant distress.
FAQs About Symptoms of Fibromyalgia Flare–Up
1. What triggers a fibromyalgia flare–up?
Common triggers include physical overexertion, stress, poor sleep, weather changes, infections, and hormonal fluctuations.
2. How long does a fibromyalgia flare–up last?
Flare–ups can last from a few days to several weeks, depending on the trigger and how quickly symptoms are addressed.
3. Are flare–ups preventable?
While not entirely preventable, flare–ups can be reduced in frequency and severity through lifestyle management, stress control, pacing, and medical support.
4. Do flare–up symptoms differ from everyday symptoms?
Yes, flare–ups usually involve a sudden increase in the intensity and range of symptoms, making daily life much harder than during baseline phases.
5. Should I see a doctor during a flare–up?
Yes, especially if symptoms are severe or unusual. A flare may also signal another underlying issue that requires medical attention.
6. Can flare–up symptoms affect mental health?
Absolutely. The physical discomfort and limitations during a flare can lead to increased anxiety, depression, and emotional instability.
Conclusion
Understanding the symptoms of a fibromyalgia flare–up is key to managing this unpredictable condition. From heightened pain and fatigue to sensory overload and emotional swings, flare–ups affect every aspect of life. By recognizing these patterns early, individuals can make adjustments, seek support, and reduce the long-term toll of fibromyalgia. While flare–ups may be an inevitable part of this chronic illness, preparation and self-awareness can empower people to navigate them with resilience and hope.