The Overlooked Link: Can Fibromyalgia Cause Low Iron in the Body?
The Overlooked Link: Can Fibromyalgia Cause Low Iron in the Body?
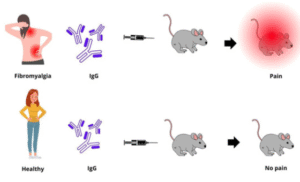
Fibromyalgia is a complex and often misunderstood condition that affects millions of individuals globally. It is primarily known for causing widespread pain, fatigue, and cognitive issues. However, a growing body of research suggests that fibromyalgia may be linked to other physiological imbalances, including low iron levels. This potential connection raises important questions about the interaction between fibromyalgia and iron metabolism.
Understanding Iron’s Role in the Body
Iron is an essential mineral required for various critical functions in the body. It plays a central role in producing hemoglobin, a component of red blood cells that carries oxygen throughout the body. Iron is also involved in energy production, immune function, and the regulation of mood and cognitive health.
Low iron levels, especially when they fall below normal but have not yet led to anemia, can still cause significant health problems. Symptoms can include fatigue, difficulty concentrating, weakness, and increased susceptibility to infections. These symptoms often overlap with those experienced by people with fibromyalgia, which makes it difficult to distinguish between the two based on clinical signs alone.
Can Fibromyalgia Lead to Low Iron?
While fibromyalgia itself may not directly cause iron deficiency, several factors associated with the condition could contribute to low iron levels.
1. Chronic Inflammation and Iron Regulation
Although fibromyalgia is not classified as an inflammatory disease in the traditional sense, there is evidence that it may involve subtle systemic inflammation. Inflammatory processes can interfere with the way the body handles iron. In particular, inflammation may increase the production of hepcidin, a hormone that blocks iron absorption and reduces the release of iron from stores in the liver. This response can lead to a state of functional iron deficiency, where iron is present in the body but unavailable for use.
2. Poor Dietary Intake and Malabsorption
Individuals with fibromyalgia often struggle with appetite changes, dietary restrictions, and gastrointestinal symptoms. These issues can lead to inadequate intake of iron-rich foods. Additionally, coexisting conditions such as irritable bowel syndrome or celiac disease may further impair the absorption of iron from the digestive tract, compounding the risk of deficiency.
3. Menstrual Blood Loss and Iron Deficiency
Women are disproportionately affected by fibromyalgia and are also more likely to experience iron deficiency due to menstrual blood loss. For those with fibromyalgia, managing heavy menstrual cycles while also dealing with chronic pain and fatigue can make it even more difficult to maintain adequate iron levels.
4. Medication Side Effects
Some medications commonly prescribed to manage fibromyalgia symptoms, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can cause gastrointestinal bleeding when used over long periods. Even minor but chronic blood loss can deplete iron stores over time, increasing the risk of iron deficiency.
Signs of Low Iron in Fibromyalgia Patients
When low iron coexists with fibromyalgia, it may amplify symptoms or create new challenges. Common signs of low iron include:
- Increased fatigue or exhaustion
- Pale skin
- Shortness of breath during mild activity
- Difficulty concentrating or brain fog
- Dizziness or lightheadedness
- Cold hands and feet
- Restless legs syndrome
Because these symptoms are also associated with fibromyalgia itself, healthcare providers may overlook iron deficiency as a contributing factor.
Testing and Diagnosis
If iron deficiency is suspected, simple blood tests can help clarify the diagnosis. Tests may include serum ferritin, hemoglobin, total iron-binding capacity (TIBC), and transferrin saturation. Ferritin is particularly important, as it reflects the body’s iron storage. Low levels of ferritin can signal a need for further evaluation and treatment, even before anemia develops.
It is essential that healthcare professionals evaluate iron status in individuals with fibromyalgia, especially those reporting increased fatigue or poor response to standard treatments. Identifying iron deficiency early can lead to more targeted interventions and improved overall well-being.
Treatment and Management Strategies
Addressing low iron in fibromyalgia patients requires a multifaceted approach. Treatment strategies may include:
- Dietary changes: Incorporating iron-rich foods such as lean meats, beans, spinach, and fortified cereals. Consuming vitamin C-rich foods alongside iron sources enhances absorption.
- Iron supplements: Oral iron supplements may be prescribed in cases of deficiency. In some instances, intravenous iron may be recommended, particularly if gastrointestinal side effects or absorption issues are present.
- Monitoring medication use: Reviewing current medications to assess the risk of gastrointestinal bleeding and adjusting as necessary under medical supervision.
- Treating underlying conditions: Addressing coexisting gastrointestinal or menstrual issues can help prevent recurring iron deficiency.
Conclusion
The question of whether fibromyalgia can cause low iron opens the door to a broader conversation about the condition’s impact on overall health. While fibromyalgia may not directly cause iron deficiency, it is clear that various aspects of the disorder—ranging from inflammation to medication use and dietary challenges—can contribute to depleted iron stores. Recognizing and addressing low iron levels in fibromyalgia patients may not only improve their physical symptoms but also enhance cognitive function and quality of life. An integrative approach that considers nutritional status alongside pain and fatigue management is essential in delivering comprehensive care for those living with fibromyalgia.