Why Do Doctors Not Treat Fibromyalgia?
Understanding the Medical Hesitation: Why Do Doctors Not Treat Fibromyalgia?
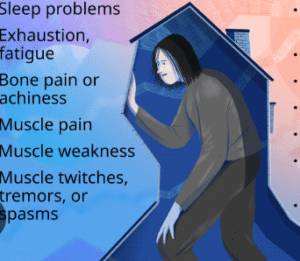
Fibromyalgia is a chronic condition characterized by widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive challenges. Despite affecting millions worldwide, it often remains underdiagnosed and inadequately treated. This raises a critical question: why do doctors not treat fibromyalgia as assertively as other chronic conditions?
The Complexity of Diagnosis
One of the primary reasons for the medical community’s hesitancy is the complexity involved in diagnosing fibromyalgia. Unlike other conditions, fibromyalgia lacks definitive laboratory tests or imaging studies for confirmation. Diagnosis primarily relies on patient-reported symptoms and the exclusion of other conditions. This subjective approach can lead to uncertainty and misdiagnosis, making some physicians reluctant to label a patient with fibromyalgia prematurely.
Lack of Comprehensive Medical Training
Many medical professionals receive limited education on fibromyalgia during their training. This gap in knowledge can result in uncertainty about the condition’s legitimacy and the best practices for management. Without a solid understanding, some doctors may feel ill-equipped to diagnose or treat fibromyalgia effectively, leading to a tendency to avoid addressing it altogether.
Perception of Fibromyalgia as a Psychological Issue
Historically, fibromyalgia has been viewed by some in the medical field as a psychosomatic disorder, primarily rooted in psychological factors rather than physiological ones. This perception can lead to skepticism about the condition’s validity, causing some doctors to dismiss symptoms or attribute them solely to mental health issues. Such attitudes can hinder appropriate treatment and support for patients.
Challenges in Treatment Efficacy
Treating fibromyalgia is notoriously challenging due to its multifaceted nature. Patients often respond variably to treatments, and what works for one individual may not work for another. The lack of universally effective treatments can be discouraging for physicians, leading some to believe that managing fibromyalgia is a futile endeavor. This belief can result in a reluctance to engage in the long-term management required for these patients.
Time Constraints in Clinical Practice
Managing fibromyalgia effectively requires a comprehensive, multidisciplinary approach, including patient education, lifestyle modifications, pharmacological interventions, and psychological support. Such an approach demands significant time and resources, which may not be feasible in busy clinical settings. Consequently, some doctors may avoid treating fibromyalgia due to the perceived time commitment involved.
Insurance and Healthcare System Limitations
Healthcare systems and insurance policies often do not provide adequate support for the multidisciplinary care fibromyalgia patients need. Limited coverage for therapies like physical therapy, counseling, or alternative treatments can restrict a physician’s ability to offer comprehensive care. These systemic barriers can discourage doctors from pursuing a fibromyalgia diagnosis or treatment plan.
Stigma and Patient-Doctor Relationships
Patients with fibromyalgia often face stigma, not only from society but sometimes from healthcare providers as well. This stigma can strain the patient-doctor relationship, leading to frustration on both sides. Doctors may feel challenged by patients who have complex, chronic symptoms without clear diagnostic markers, leading to a breakdown in communication and trust.
Evolving Understanding and Future Directions
Despite these challenges, the medical community’s understanding of fibromyalgia is evolving. Research is shedding light on the neurological and physiological underpinnings of the condition, leading to more effective treatment strategies. Educational initiatives are also being implemented to improve physician awareness and competence in managing fibromyalgia.
Conclusion
The question of why doctors do not treat fibromyalgia adequately is multifaceted, involving diagnostic complexities, educational gaps, systemic healthcare limitations, and societal stigma. Addressing these issues requires a concerted effort to enhance medical education, reform healthcare policies, and foster a more empathetic and informed approach to patient care. As our understanding of fibromyalgia continues to grow, so too does the potential for more effective and compassionate treatment strategies.