The Hidden Strain: What Is Fibromyalgia Leg Pain Like and Why It Matters
Understanding Fibromyalgia and Its Impact on the Legs
Fibromyalgia is a chronic condition that affects the nervous system, muscles, and soft tissues, producing a variety of symptoms including widespread pain, fatigue, cognitive issues, and sleep disturbances. One of the more persistent and troubling symptoms reported by individuals with fibromyalgia is leg pain. This type of pain can manifest in different ways and significantly impacts daily life, mobility, and mental health.
Leg pain in fibromyalgia is not caused by an injury or inflammation, but rather by an abnormal response to pain in the central nervous system. People with fibromyalgia have a heightened sensitivity to pain, which means that even minor discomfort in the muscles, tendons, or nerves can feel intense. Understanding what this pain feels like, where it occurs, and why it happens is essential to managing the condition more effectively.
Describing the Sensation of Fibromyalgia Leg Pain
The pain experienced in the legs due to fibromyalgia is often described in a variety of ways depending on the individual and the severity of their condition. Common sensations include:
- A deep, throbbing ache that can feel like it originates from the bones or deep muscle tissue
- Burning sensations that may move from the thighs to the calves
- A sharp, stabbing feeling that comes and goes unpredictably
- Tingling or a sensation similar to pins and needles, sometimes mistaken for nerve damage
- Cramping in the calves, particularly at night or after long periods of sitting or standing
The intensity of the pain can range from a dull discomfort to an overwhelming and incapacitating sensation. In many cases, it is accompanied by muscle stiffness, especially in the morning or after rest. For some individuals, the pain worsens with physical activity, stress, cold temperatures, or lack of sleep.
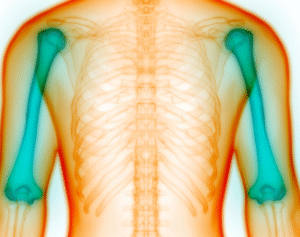
Locations of Pain in the Legs
Fibromyalgia-related leg pain can occur in any part of the lower limbs, but there are some areas more commonly affected:
- Thighs: Often feel sore or deeply fatigued, as if the muscles have been overused
- Calves: Frequently experience cramping or burning sensations
- Knees: May feel tender or unstable, although there’s no joint inflammation
- Feet and Ankles: Can develop a painful tingling or numbing sensation, especially after extended activity or pressure
The pain may present symmetrically, affecting both legs equally, or may be more pronounced on one side depending on movement patterns, posture, or individual flare-ups.
Leg Pain vs. Restless Leg Syndrome
It is important to differentiate fibromyalgia leg pain from similar conditions such as restless leg syndrome (RLS). While both can occur simultaneously in some patients, they are distinct issues. RLS is characterized by an uncontrollable urge to move the legs due to uncomfortable sensations, particularly in the evening or at night. Fibromyalgia leg pain, however, can happen any time and does not always involve the need to move. The sensations with fibromyalgia are often more deeply rooted and can include a combination of aching, burning, and fatigue that feels muscular in nature.
Impact on Mobility and Daily Activities
Leg pain in fibromyalgia can interfere significantly with daily tasks. Walking, climbing stairs, standing for extended periods, or even sitting in one position too long can trigger or worsen symptoms. This reduced physical function can lead to a sedentary lifestyle, which may increase stiffness and further muscle discomfort. Additionally, limited mobility may contribute to feelings of frustration, isolation, and depression, creating a negative cycle that exacerbates symptoms.
What Triggers or Worsens Fibromyalgia Leg Pain
Several factors can intensify leg pain in individuals with fibromyalgia, including:
- Physical exertion or overuse of muscles
- Cold or damp weather conditions
- Poor quality sleep or sleep disturbances
- Emotional stress or anxiety
- Hormonal fluctuations
- Poor posture or improper footwear
Awareness of these triggers can help patients anticipate and reduce the severity of pain through proactive strategies and lifestyle modifications.
Effective Strategies for Managing Leg Pain
While fibromyalgia currently has no cure, several strategies have shown to be effective in alleviating leg pain:
- Gentle Exercise: Low-impact activities such as swimming, yoga, or walking can improve circulation, flexibility, and muscle endurance without overexertion.
- Heat Therapy: Warm baths, heating pads, or thermal wraps can help relax tight muscles and relieve pain.
- Massage Therapy: Gentle massage can reduce tension and promote relaxation, though it should be performed by professionals familiar with fibromyalgia.
- Stretching: Regular, mild stretching of the legs can help maintain range of motion and reduce stiffness.
- Sleep Hygiene: Establishing a consistent sleep schedule and a calming bedtime routine can reduce flare-ups related to sleep deprivation.
- Medication: Some individuals benefit from prescribed medications that help regulate pain perception, such as certain antidepressants or anticonvulsants.
Long-Term Outlook for Those with Fibromyalgia Leg Pain
Living with fibromyalgia leg pain can be challenging, but with the right combination of self-care, professional treatment, and support, individuals can improve their quality of life. Pain management techniques continue to evolve, and ongoing research into the neurological underpinnings of fibromyalgia holds promise for more effective treatments in the future. Staying proactive and informed empowers those affected to navigate their condition more confidently and comfortably.
Frequently Asked Questions
1. What does fibromyalgia leg pain feel like?
It often feels like a deep ache, burning, or sharp stabbing pain, sometimes accompanied by tingling or cramping in the thighs, calves, or feet.
2. Is fibromyalgia leg pain constant or does it come and go?
It can vary from person to person. Some experience it constantly, while others have flare-ups triggered by specific activities or stressors.
3. Can fibromyalgia cause leg weakness?
Yes, some individuals report feeling weakness or instability in the legs, although this is usually due to muscle fatigue rather than actual nerve damage.
4. Does exercise help or worsen fibromyalgia leg pain?
Mild, consistent exercise usually helps reduce symptoms, but overexertion can trigger flare-ups, so balance and moderation are key.
5. How can I sleep better with fibromyalgia leg pain?
Using supportive pillows, practicing relaxation techniques, maintaining a regular sleep schedule, and using heat therapy before bed may help improve sleep.
6. Are there specific medications for leg pain in fibromyalgia?
Some medications, including duloxetine, pregabalin, or amitriptyline, may help manage widespread pain and are often prescribed to fibromyalgia patients under a doctor’s supervision.