Unmasking the Origins of Fibromyalgia: A Comprehensive Exploration of Its Root Causes
Unmasking the Origins of Fibromyalgia: A Comprehensive Exploration of Its Root Causes
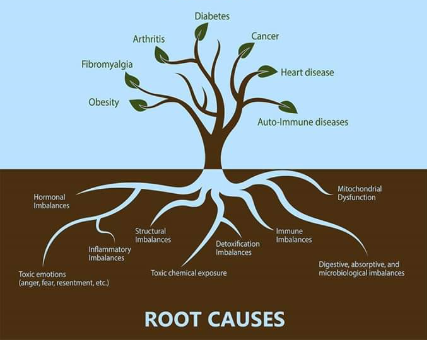
Fibromyalgia is a chronic condition characterized by widespread musculoskeletal pain, fatigue, and cognitive disturbances. Despite extensive research, its exact cause remains elusive. However, current studies suggest that fibromyalgia results from a combination of factors affecting the central nervous system, genetics, environmental triggers, and psychological stressors.
Central Nervous System Sensitization
One prevailing theory is that fibromyalgia stems from central sensitization, where the central nervous system (CNS) becomes hypersensitive to pain signals. This heightened sensitivity leads to an amplified perception of pain, even in response to non-painful stimuli. Functional MRI studies have shown altered brain activity in regions responsible for pain processing in individuals with fibromyalgia.
Neurochemical Imbalances
Research indicates that people with fibromyalgia may have abnormal levels of certain neurotransmitters, such as serotonin, dopamine, and norepinephrine, which play roles in mood regulation and pain perception. Additionally, elevated levels of substance P, a neuropeptide associated with pain transmission, have been found in the cerebrospinal fluid of fibromyalgia patients.
Genetic Predisposition
Genetics may contribute to fibromyalgia susceptibility. Studies have identified familial patterns, suggesting a hereditary component. Specific gene polymorphisms related to serotonin transport and catechol-O-methyltransferase (COMT) enzymes have been associated with increased risk, although no single gene has been pinpointed as the definitive cause.
Environmental and Physical Triggers
Certain environmental factors and physical traumas are known to trigger or exacerbate fibromyalgia symptoms. These include:
- Infections (e.g., Epstein-Barr virus, Lyme disease)
- Physical injuries or surgeries
- Exposure to stressful or traumatic events
- Chronic sleep disturbances
- Such events may initiate or intensify the central sensitization process, leading to the development or worsening of fibromyalgia symptoms.
Psychological Stress and Trauma
Psychological factors, including chronic stress, anxiety, and post-traumatic stress disorder (PTSD), have been linked to fibromyalgia. Emotional trauma can alter pain perception and stress response systems, potentially contributing to the onset and persistence of fibromyalgia symptoms.
Sleep Disorders
Non-restorative sleep is a common complaint among fibromyalgia patients. Sleep disturbances can exacerbate pain sensitivity and fatigue, creating a vicious cycle that perpetuates the condition. The relationship between sleep disorders and fibromyalgia suggests that disrupted sleep may play a role in its pathogenesis.
Hormonal and Endocrine Factors
Abnormalities in the hypothalamic-pituitary-adrenal (HPA) axis, which regulates stress responses, have been observed in fibromyalgia patients. Altered cortisol levels and other hormonal imbalances may influence pain perception and stress tolerance, contributing to symptom development.
Immune System Involvement
Emerging research suggests that immune system dysregulation may be involved in fibromyalgia. Elevated levels of pro-inflammatory cytokines have been detected in some patients, indicating a potential link between immune responses and chronic pain. However, more studies are needed to clarify this relationship.
Conclusion
Fibromyalgia is a multifactorial condition with no single identifiable cause. Its development likely involves an interplay of central nervous system sensitization, neurochemical imbalances, genetic predisposition, environmental triggers, psychological stress, sleep disturbances, hormonal factors, and immune system involvement. Understanding these contributing factors is essential for developing effective treatment strategies and improving patient outcomes.