Unveiling the Diagnostic Path: What Confirms Fibromyalgia?
Introduction
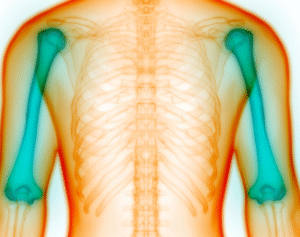
Fibromyalgia is a chronic condition characterized by widespread musculoskeletal pain, fatigue, and tenderness in localized areas. Diagnosing fibromyalgia can be challenging due to the absence of specific laboratory tests and the overlap of its symptoms with other disorders. This article delves into the established criteria and methodologies that healthcare professionals employ to confirm a fibromyalgia diagnosis.
Understanding Fibromyalgia Diagnosis
The diagnosis of fibromyalgia is primarily clinical, relying on patient-reported symptoms and physical examination findings. Over the years, various criteria have been developed to aid in the accurate identification of this condition.
American College of Rheumatology (ACR) Criteria
The ACR has established criteria to standardize the diagnosis of fibromyalgia. The 2016 revision emphasizes the following:
- Widespread Pain Index (WPI): Patients report pain in at least 4 of 5 regions, encompassing 19 specific body areas.
- Symptom Severity Scale (SSS): Assessment of fatigue, unrefreshed sleep, cognitive symptoms, and somatic symptoms, each rated on a scale from 0 to 3
- Duration: Symptoms must be present at a similar level for at least three months.
- Exclusion of Other Conditions: No other disorder should explain the symptoms.
A diagnosis is confirmed if the WPI is ≥7 and the SSS is ≥5, or if the WPI is between 4–6 and the SSS is ≥9.
Diagnosis of Exclusion
Given the nonspecific nature of fibromyalgia symptoms, it’s crucial to rule out other conditions that may mimic its presentation. Healthcare providers often conduct comprehensive evaluations, including laboratory tests and imaging studies, to exclude disorders such as rheumatoid arthritis, lupus, and hypothyroidism.
Role of Specialists
While primary care physicians can initiate the diagnostic process, rheumatologists are often involved due to their expertise in musculoskeletal disorders. Their specialized knowledge aids in differentiating fibromyalgia from other rheumatic diseases.
Conclusion
Confirming a fibromyalgia diagnosis involves a meticulous assessment of symptoms, adherence to established criteria, and the exclusion of other potential conditions. Understanding the diagnostic process empowers patients to seek appropriate care and manage their symptoms effectively.
Frequently Asked Questions
1. Can fibromyalgia be diagnosed through blood tests?
No, there are no specific blood tests for fibromyalgia. However, tests may be conducted to rule out other conditions.
2. Is the tender point test still used for diagnosis?
The tender point test has been largely replaced by the ACR’s 2016 criteria, which focus on widespread pain and symptom severity.
3. How long must symptoms persist for a fibromyalgia diagnosis?
Symptoms should be present at a similar level for at least three months.
4. Can fibromyalgia coexist with other conditions?
Yes, fibromyalgia can coexist with other disorders, but it’s essential to ensure that symptoms are not solely attributable to another condition.
5. Who is best qualified to diagnose fibromyalgia?
While primary care physicians can diagnose fibromyalgia, rheumatologists have specialized expertise in musculoskeletal disorders and are often involved in the diagnostic process.
6. Are imaging studies useful in diagnosing fibromyalgia?
Imaging studies are not used to diagnose fibromyalgia directly but may be employed to exclude other conditions.