Unraveling the Viral Connection: Exploring the Role of Infections in Fibromyalgia
Understanding Fibromyalgia and Its Complex Origins
Fibromyalgia is a chronic disorder characterized by widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive difficulties. Despite extensive research, the exact cause of fibromyalgia remains elusive. However, various factors, including genetic predisposition, environmental influences, and infections, have been implicated in its onset.
The Potential Viral Triggers of Fibromyalgia
Several viral infections have been associated with the development or exacerbation of fibromyalgia symptoms. While a direct causal relationship has not been definitively established, the following viruses are frequently mentioned in medical literature:
- Epstein-Barr Virus (EBV): Known for causing mononucleosis, EBV has been observed in higher prevalence among individuals with fibromyalgia. Some studies suggest that EBV may trigger fibromyalgia symptoms in susceptible individuals.
- Hepatitis C Virus (HCV): Chronic HCV infection has been linked to musculoskeletal pain and fatigue, symptoms commonly seen in fibromyalgia. The overlap in symptoms has led researchers to explore a potential connection between HCV and fibromyalgia.
- Human Immunodeficiency Virus (HIV): Individuals with HIV may experience chronic pain and fatigue, leading to investigations into the relationship between HIV infection and fibromyalgia-like symptoms.
- Herpesviruses: Certain herpesviruses, such as Human Herpesvirus 6 (HHV-6) and Cytomegalovirus (CMV), have been studied for their potential role in fibromyalgia. These viruses can remain dormant in the body and may reactivate under certain conditions, possibly contributing to symptom flare-ups.
- SARS-CoV-2 (COVID-19): The emergence of COVID-19 has brought attention to post-viral syndromes, with some individuals experiencing prolonged symptoms resembling fibromyalgia. This has prompted further research into the long-term effects of viral infections on chronic pain conditions.
Mechanisms Linking Viral Infections to Fibromyalgia
The exact mechanisms by which viral infections may contribute to fibromyalgia are not fully understood. However, several hypotheses have been proposed:
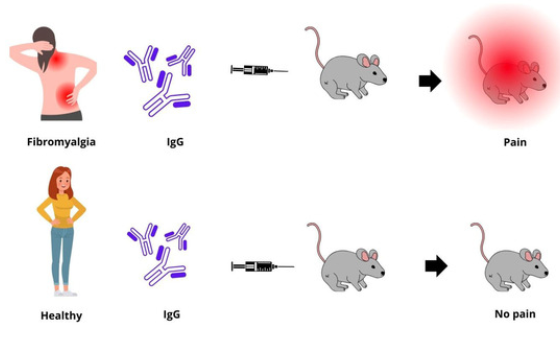
- Immune System Dysregulation: Viral infections can lead to persistent immune activation or dysregulation, potentially resulting in chronic inflammation and heightened pain sensitivity.
- Neuroinflammation: Some viruses may cause inflammation in the central nervous system, affecting pain processing pathways and leading to symptoms associated with fibromyalgia.
- Mitochondrial Dysfunction: Viral infections might impair mitochondrial function, leading to decreased energy production and increased fatigue, a hallmark of fibromyalgia.
- Genetic Susceptibility: Individuals with certain genetic profiles may be more prone to developing fibromyalgia following a viral infection, suggesting an interplay between genetics and environmental triggers.
Current Research and Future Directions
Ongoing research aims to clarify the relationship between viral infections and fibromyalgia. Studies are exploring biomarkers that could identify individuals at risk, as well as potential antiviral treatments that may alleviate symptoms. Understanding the role of viruses in fibromyalgia could lead to more targeted therapies and improved patient outcomes.
Conclusion
While a definitive link between specific viruses and fibromyalgia has not been conclusively established, evidence suggests that viral infections may act as triggers in susceptible individuals. Further research is necessary to unravel the complex interactions between viral agents, the immune system, and chronic pain pathways. Recognizing the potential role of infections in fibromyalgia underscores the importance of a comprehensive approach to diagnosis and treatment.
Frequently Asked Questions
1. Can a viral infection directly cause fibromyalgia?
While viral infections are not proven to directly cause fibromyalgia, they may act as triggers in individuals with genetic or environmental predispositions.
2. Are there specific viruses more commonly associated with fibromyalgia?
Viruses such as Epstein-Barr Virus, Hepatitis C, HIV, and certain herpesviruses have been studied for their potential links to fibromyalgia symptoms.
3. How do viral infections contribute to fibromyalgia symptoms?
Viral infections may lead to immune system changes, neuroinflammation, and mitochondrial dysfunction, all of which can contribute to the development or exacerbation of fibromyalgia symptoms.
4. Is there a test to determine if a viral infection has triggered fibromyalgia?
Currently, there is no specific test to confirm a viral trigger for fibromyalgia. Diagnosis is based on clinical evaluation and ruling out other conditions.
5. Can antiviral treatments help manage fibromyalgia symptoms?
Research is ongoing to determine the efficacy of antiviral treatments in fibromyalgia management. Some studies suggest potential benefits, but more evidence is needed.
6. Should individuals with a history of viral infections be monitored for fibromyalgia?
Individuals with persistent symptoms following a viral infection should consult healthcare providers for evaluation, as early intervention may improve outcomes.