The Silent Intersection: Exploring Whether Fibromyalgia Weakens Bones Over Time
Fibromyalgia is often described as an invisible illness, marked by widespread musculoskeletal pain, fatigue, and cognitive disturbances. While the primary concern revolves around nerve sensitivity and chronic pain, a growing number of patients and healthcare professionals have questioned whether fibromyalgia has a more far-reaching impact on the body, including on the bones. The central question remains: does fibromyalgia weaken bones?
To address this question, it is essential to distinguish between the direct and indirect effects of fibromyalgia. While fibromyalgia does not directly cause bone deterioration or loss of bone density in the same way that conditions like osteoporosis do, it can create circumstances that negatively influence bone health over time. These indirect impacts, when left unaddressed, could lead to weakening of bones and higher risk of fractures.
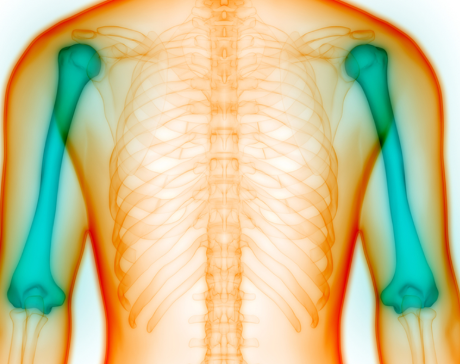
Reduced Physical Activity and Bone Health
One of the key factors influencing bone strength is regular weight-bearing physical activity. Individuals with fibromyalgia often experience persistent pain and fatigue, leading to a sedentary lifestyle. This decrease in physical activity can result in muscle atrophy and lower mechanical stress on bones, both of which are essential stimuli for maintaining healthy bone density.
Bones are dynamic structures that respond to regular movement and pressure. Lack of consistent exercise, particularly weight-bearing activities like walking or resistance training, can lead to demineralization and reduced bone strength over time. Thus, while fibromyalgia does not inherently weaken bones, the inactivity that often accompanies the condition can certainly contribute to this decline.
The Role of Sleep and Hormonal Imbalance
Chronic sleep disturbances are a hallmark of fibromyalgia. Sleep plays a critical role in tissue repair, hormonal regulation, and overall musculoskeletal maintenance. Disrupted sleep patterns may impair the body’s ability to produce hormones that regulate calcium absorption and bone remodeling.
Hormonal imbalances, such as lower levels of growth hormone or abnormalities in cortisol production, have been observed in some people with fibromyalgia. These disruptions may affect the delicate balance of bone formation and resorption, increasing the risk of weakened bones indirectly.
Nutritional Deficiencies in Fibromyalgia Patients
Many individuals with fibromyalgia struggle to maintain a nutritious diet due to symptoms like nausea, irritable bowel syndrome, or appetite loss. Over time, this may lead to deficiencies in key nutrients that support bone health, such as calcium, vitamin D, magnesium, and phosphorus.
Vitamin D, in particular, is vital for calcium absorption and bone strength. Low levels of vitamin D are commonly reported among fibromyalgia patients. Without sufficient vitamin D, bones can become brittle and more prone to fractures. Similarly, inadequate calcium intake further compounds this issue, creating a scenario where bone health deteriorates not because of fibromyalgia itself but due to secondary consequences of the condition.
Medication Side Effects and Bone Density
Certain medications commonly prescribed to manage fibromyalgia symptoms, including corticosteroids and selective serotonin reuptake inhibitors (SSRIs), have been associated with reduced bone mineral density. Prolonged use of corticosteroids, in particular, is a known risk factor for osteoporosis.
While not every fibromyalgia patient will use these medications long-term, it is an important consideration. Individuals relying on pharmacological interventions for extended periods should discuss bone health monitoring with their healthcare providers.
Stress and Bone Health Connection
Chronic stress is another common feature in fibromyalgia. Elevated levels of stress hormones like cortisol have been linked to decreased bone formation and increased bone resorption. Over time, this can tip the balance toward bone loss. People with fibromyalgia often live with a constant undercurrent of physiological stress, which could, in the long run, influence the strength and integrity of their bones.
Preventative Measures for Protecting Bone Strength
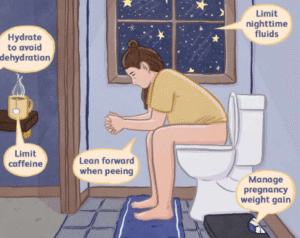
While fibromyalgia may not directly weaken bones, those living with the condition should still be proactive in supporting skeletal health. This includes incorporating safe and gentle weight-bearing exercises, such as walking, tai chi, or light resistance training, into their daily routine.
Dietary attention is also crucial. Ensuring adequate intake of calcium-rich foods and vitamin D, whether through sunlight exposure or supplements, plays a significant role. Regular blood work can help identify deficiencies early on.
Additionally, stress management techniques like deep breathing, meditation, and cognitive behavioral therapy can lower cortisol levels and potentially reduce the burden on bone metabolism.
Conclusion
Fibromyalgia does not directly cause weakened bones, but its indirect effects, such as decreased physical activity, poor sleep, hormonal imbalances, nutritional deficiencies, and long-term medication use, can all contribute to compromised bone health over time. Understanding these links provides individuals with fibromyalgia the opportunity to make informed choices that protect and preserve bone strength.
Addressing these risk factors early, under the guidance of a healthcare provider, ensures that the complications commonly associated with sedentary behavior and poor nutrient absorption do not evolve into more serious musculoskeletal conditions. Bone health should be viewed as an integral component of fibromyalgia care, and preventative strategies must be a part of any long-term treatment plan.
Frequently Asked Questions
1. Can fibromyalgia directly cause osteoporosis?
No, fibromyalgia does not directly lead to osteoporosis, but inactivity and medication side effects may increase the risk.
2. Is vitamin D important for fibromyalgia patients?
Yes, vitamin D supports bone health and may also help manage fibromyalgia symptoms like pain and fatigue.
3. What kind of exercise is safe for fibromyalgia and bone health?
Gentle, low-impact exercises such as walking, yoga, or swimming are safe and beneficial for both fibromyalgia and bone strength.
4. Should fibromyalgia patients take calcium supplements?
Only under medical guidance, as too much calcium can have adverse effects. A balanced diet is the best approach.
5. Are SSRIs safe for long-term use in fibromyalgia patients with bone concerns?
They are generally safe, but patients should be monitored for bone density loss if used long-term.
6. How can I know if my bones are weakening?
A bone density scan, known as a DEXA scan, can assess bone strength and detect early signs of osteoporosis.