How Does Fibromyalgia Affect the Nervous System?
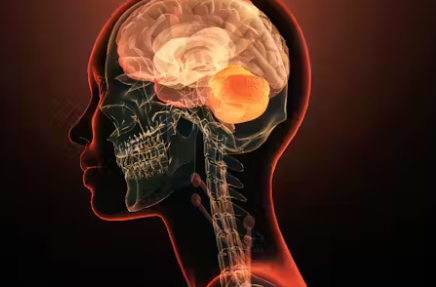
Fibromyalgia is a chronic and complex disorder that has long puzzled both patients and healthcare professionals. Characterized by widespread musculoskeletal pain, fatigue, and cognitive issues, fibromyalgia is increasingly recognized as a condition with deep neurological roots. Understanding how fibromyalgia affects the nervous system offers critical insights into why the symptoms are so varied and often misunderstood.
Unlike conditions that stem from visible damage or inflammation, fibromyalgia’s effects on the nervous system are more subtle yet widespread. They involve alterations in pain processing, neurotransmitter imbalances, nerve sensitivity, and dysfunctions in both the central and peripheral nervous systems. This combination creates a cascade of symptoms that can significantly impair quality of life.
Central Sensitization: The Core Mechanism
At the heart of fibromyalgia lies a phenomenon called central sensitization. This refers to an increased responsiveness of neurons in the central nervous system, especially in the spinal cord and brain, to sensory input. In simpler terms, the nervous system becomes hyper-alert and overreacts to pain signals.
Even light touch, mild pressure, or temperature changes may be perceived as painful. The brain fails to properly regulate pain perception, leading to amplified sensations that would not normally cause discomfort. This miscommunication is not due to psychological factors but rather a measurable dysfunction in neural pathways.
Neurotransmitter Imbalances
Fibromyalgia patients often show irregular levels of certain brain chemicals that transmit signals across nerves. These include:
- Serotonin: Often reduced in fibromyalgia, which can contribute to pain sensitivity, mood disorders, and poor sleep
- Dopamine: Involved in motivation and reward, its deficiency may relate to fatigue and anhedonia
- Substance P: Found in higher levels in cerebrospinal fluid, this peptide intensifies pain signals
- Norepinephrine: A key player in the body’s stress response, its imbalance can worsen anxiety and alertness issues
These chemical imbalances create a nervous system that is constantly on edge, unable to regulate itself properly, and prone to misinterpreting benign signals as threats.
Peripheral Nerve Dysfunction
While the central nervous system plays a dominant role, emerging research also points to peripheral nerve abnormalities in some fibromyalgia patients. These nerves, located outside the brain and spinal cord, help relay sensations from the skin, muscles, and joints to the brain.
In fibromyalgia, small fiber neuropathy has been identified in a subset of individuals. This refers to damage or dysfunction in the tiny nerve fibers responsible for pain and temperature sensation. Symptoms of this condition may include:
- Burning or tingling sensations
- Hypersensitivity to touch
- Cold intolerance
- Numbness or poor coordination
Although not present in every case, this evidence suggests that fibromyalgia may, in part, involve physical nerve damage or misfiring at the peripheral level.
Autonomic Nervous System and Dysregulation
The autonomic nervous system (ANS) controls involuntary body functions like heart rate, digestion, and temperature regulation. In fibromyalgia, many individuals show signs of autonomic dysfunction, sometimes called dysautonomia. This manifests as:
- Rapid heartbeat or palpitations
- Dizziness upon standing
- Temperature sensitivity
- Digestive issues like bloating and constipation
- Night sweats or excessive sweating
These symptoms arise from the body’s inability to maintain balance between the sympathetic (fight-or-flight) and parasympathetic (rest-and-digest) branches of the nervous system. The result is a state of chronic imbalance that can worsen fatigue and pain perception.
Cognitive Impairment and the Brain
Another critical neurological feature of fibromyalgia is the impact on cognitive function, often referred to as fibro fog. This can affect various domains of mental processing, including:
- Short-term memory
- Concentration and attention span
- Word retrieval and language use
- Decision-making speed
- Multitasking ability
Brain imaging studies have shown that people with fibromyalgia exhibit changes in brain structure and function. Areas responsible for pain processing, memory, and emotional regulation, such as the prefrontal cortex and hippocampus, may display reduced volume or altered connectivity.
These findings suggest that fibromyalgia is not just a disorder of sensation but also of cognition, rooted in real and observable changes in brain activity.
Sleep Disruption and Nervous System Repercussions
Poor sleep is both a symptom and a contributor to nervous system dysfunction in fibromyalgia. People with this condition often experience non-restorative sleep, frequent awakenings, and even sleep disorders like restless legs syndrome or sleep apnea.
Sleep is vital for nervous system repair and neurotransmitter regulation. Chronic sleep deprivation can exacerbate central sensitization, heighten pain perception, and worsen cognitive function. It creates a vicious cycle where nervous system dysfunction leads to poor sleep, which in turn deepens neurological impairment.
Sensory Overload and Hypersensitivity
The nervous system in fibromyalgia is unusually reactive to external stimuli. Individuals may become overwhelmed by:
- Bright lights
- Loud sounds
- Strong smells
- Textures or fabrics on the skin
This heightened sensory processing reflects a breakdown in the brain’s ability to filter irrelevant or non-threatening stimuli. It leads to a constant sense of overload, contributing to anxiety, irritability, and mental fatigue.
This form of sensory hypersensitivity is not psychosomatic. Rather, it demonstrates how the nervous system, when dysregulated, can fail to protect against information overload and stress.
Chronic Stress and the Nervous System
Living with fibromyalgia means living with an overactive stress response. The nervous system remains in a state of hypervigilance, even in the absence of real danger. Over time, this can exhaust the body’s natural stress-regulation systems and impair healing.
The hypothalamic-pituitary-adrenal (HPA) axis, which governs stress hormone release, may become dysfunctional. Irregular cortisol levels can affect sleep, inflammation, and emotional stability. This chronic state of nervous tension adds a layer of weariness to an already burdened system.
FAQs About How Fibromyalgia Affects the Nervous System
1. Is fibromyalgia a neurological disease?
While not classified strictly as a neurological disorder, fibromyalgia involves significant dysfunction in the nervous system, especially in pain and sensory processing.
2. Can fibromyalgia cause nerve damage?
Some individuals with fibromyalgia show signs of small fiber neuropathy, a type of peripheral nerve damage, but it is not present in all cases.
3. Why is my body so sensitive to pain and touch with fibromyalgia?
Central sensitization causes the brain and spinal cord to amplify pain signals, making even gentle stimuli feel painful.
4. Does fibromyalgia affect brain function?
Yes, cognitive impairments like memory loss and difficulty concentrating are common, and brain imaging has shown changes in neural activity and structure.
5. How does the autonomic nervous system play a role in fibromyalgia?
Dysfunction in this system can lead to symptoms like rapid heartbeat, digestive issues, and poor temperature regulation, commonly seen in fibromyalgia patients.
6. Can fibromyalgia be treated by targeting the nervous system?
Yes, many treatments aim to calm nerve activity, including medications like antidepressants and anticonvulsants, as well as non-drug therapies such as biofeedback and mindfulness.
Conclusion
Fibromyalgia’s impact on the nervous system is both profound and multifaceted. From disrupted pain signals and neurotransmitter imbalances to cognitive fog and autonomic dysfunction, this condition reveals the delicate balance required for healthy nerve function. Recognizing fibromyalgia as a neurological condition allows for better diagnosis, improved treatment strategies, and more compassionate care.
Living with fibromyalgia is a daily negotiation with an overactive and sensitive nervous system. But with proper management, education, and support, individuals can regain control, improve function, and live a more balanced life despite the challenges posed by this invisible condition.
Leave a Reply